Artificial Cornea: Engineering Advancements in Medical Artificial Organs
The field of biomedical engineering has witnessed remarkable progress over the years, particularly in the development of artificial organs. One such significant advancement is the creation of an artificial cornea, a revolutionary solution for individuals suffering from corneal blindness. Imagine a world where those affected by this debilitating condition could regain their vision and experience the beauty of the surrounding environment once again. This article delves into the cutting-edge research and developments in engineering that have led to the emergence of artificial corneas as a viable alternative for patients awaiting traditional corneal transplants.
Corneal blindness affects millions globally, posing challenges to both patients and medical professionals alike. Traditional treatments such as corneal transplantation often face limitations due to scarcity of donor tissue and potential complications associated with immune rejection. However, recent advancements in biomaterials, tissue engineering techniques, and surgical procedures have paved the way for a new era in ophthalmology – one where engineered artificial corneas offer renewed hope and possibilities. By analyzing case studies and exploring key technological breakthroughs, this article aims to shed light on how these innovative solutions are transforming lives while highlighting areas that warrant further investigation for continued improvement in artificial organ technology.
The Need for Artificial Cornea
The loss of vision due to corneal diseases or injuries can significantly impact an individual’s quality of life. Traditional treatments, such as corneal transplantation, have limitations in terms of availability and compatibility. As a result, the development of artificial corneas has emerged as a promising solution to address this unmet medical need.
To illustrate the importance of artificial corneas, consider the case of Sarah, a 45-year-old woman suffering from keratoconus—a progressive thinning of the cornea that distorts her vision. Despite wearing contact lenses, she experiences significant visual impairment and discomfort on a daily basis. Unfortunately, due to limited donor tissue availability and potential complications associated with transplantation surgery, Sarah is not a suitable candidate for traditional corneal transplant.
In light of cases like Sarah’s and numerous others worldwide facing similar challenges, it becomes evident that there is an urgent need for advancements in the field of artificial corneas. To further emphasize this point:
- Patients’ physical well-being: Without proper vision correction, individuals experience difficulties in performing everyday tasks such as reading, driving, or recognizing faces.
- Psychological impact: Visual impairment often leads to decreased self-esteem, social isolation, and depression.
- Economic burden: Costs associated with long-term treatment plans including medications and frequent doctor visits add financial strain on patients and healthcare systems alike.
- Limited accessibility: Availability of donor tissues varies across different regions globally. Moreover, certain populations face cultural or religious barriers towards accepting donated organs.
| Patients’ Physical Well-being | Psychological Impact | Economic Burden | Limited Accessibility |
|---|---|---|---|
| Difficulties in daily tasks | Decreased self-esteem | Financial strain | Varying global availability |
| Impaired functionality | Social isolation | Increased healthcare costs | Cultural/religious barriers |
| Reduced quality of life | Depression | Inadequate insurance coverage |
In light of these challenges, researchers and engineers have been diligently working to develop an artificial cornea that can restore vision effectively. The subsequent section will delve into the intricate structure of the cornea, providing a deeper understanding of its composition and function.
Understanding the Structure of the Cornea
The cornea is a vital part of our visual system, responsible for refracting and focusing light onto the retina. To fully comprehend how artificial corneas can effectively restore vision, it is crucial to delve into the intricate structure of this remarkable tissue.
One example that highlights the significance of understanding corneal structure is keratoconus, a progressive eye disorder characterized by thinning and bulging of the cornea. In this condition, the irregular shape of the cornea distorts vision and affects daily life activities such as reading or driving. By comprehending its complex structure, researchers have been able to develop innovative treatment options like intrastromal ring segments or customized contact lenses to improve visual acuity in keratoconus patients.
To better understand the structural intricacies of the cornea, let’s explore its key components:
- Epithelium: The outermost layer acts as a protective barrier against foreign particles and infection.
- Bowman’s Layer: Located beneath the epithelium, this strong layer provides structural support.
- Stroma: Comprising around 90% of the total thickness, this layer consists of collagen fibers arranged in an organized lattice, contributing to transparency.
- Endothelium: The innermost layer maintains hydration levels within the cornea through a delicate pumping mechanism.
| Component | Function |
|---|---|
| Epithelium | Protection against external elements |
| Bowman’s Layer | Structural support |
| Stroma | Maintenance of transparency |
| Endothelium | Regulating hydration levels within the cornea |
Understanding these distinct layers and their functions not only aids in identifying potential targets for developing artificial corneas but also guides researchers towards creating biomimetic materials capable of replicating their properties accurately.
Transitioning seamlessly from our exploration of corneal structure, we now move on to the next section, where we will delve into the advancements in corneal tissue engineering. By building upon this foundational knowledge of corneal structure, researchers have made significant strides towards developing artificial corneas that closely mimic their natural counterparts.
Advancements in Corneal Tissue Engineering
The cornea is a transparent, dome-shaped tissue located at the front of the eye. It plays a crucial role in vision by refracting light and focusing it onto the retina. To comprehend advancements in corneal tissue engineering, it is essential to delve into the structure of this remarkable organ.
To illustrate its complex composition, consider a hypothetical scenario where an individual suffers from corneal damage due to injury. In this case, the various layers of the cornea would be affected differently. The outermost layer, called the epithelium, acts as a protective barrier against external agents such as dust or bacteria. Beneath it lies Bowman’s layer, which provides structural support and aids in maintaining shape. The stroma occupies most of the cornea’s thickness and consists primarily of collagen fibers arranged in a precise lattice pattern for optimal transparency. Finally, Descemet’s membrane serves as another layer of protection before reaching the inner endothelium responsible for regulating fluid balance within the cornea.
With an understanding of its intricate structure, researchers have made significant progress towards developing artificial corneas using tissue engineering techniques. These advancements aim to address issues such as donor shortage and rejection often associated with traditional corneal transplantation methods.
One approach involves utilizing bioengineered scaffolds that mimic the natural architecture of the cornea to guide cell growth and regeneration. These scaffolds are typically composed of biocompatible materials like synthetic polymers or decellularized human tissues. By providing a three-dimensional framework similar to native corneal tissue, they facilitate cell attachment and organization during tissue formation.
Furthermore, scientists have explored incorporating stem cells into these engineered constructs to enhance their regenerative potential. Stem cells possess unique properties that allow them to differentiate into specialized cell types found in different layers of the cornea. This breakthrough has opened new avenues for cultivating functional replacement tissues, offering hope to individuals suffering from corneal diseases or injuries.
Emotional Response:
- Enhanced quality of life for patients with corneal damage
- Reduction in the wait time for corneal transplants due to donor shortage
- Improved success rates and long-term outcomes of artificial cornea transplantation
| Emotional Responses |
|---|
| Increased Hope |
| Restored Vision |
| Reduced Anxiety |
| Improved Quality of Life |
Continuing these advancements, researchers have been exploring innovative materials that can further improve artificial corneas’ performance. By carefully selecting appropriate materials, scientists aim to enhance biocompatibility, optical clarity, and mechanical stability. This allows for better integration within the eye and improved visual outcomes for patients.
Transitioning into the subsequent section about “Innovative Materials for Artificial Cornea,” these developments highlight the ongoing efforts in creating a more effective solution towards restoring vision and revolutionizing ophthalmology.
Innovative Materials for Artificial Cornea
Advancements in Corneal Tissue Engineering have paved the way for innovative materials to be utilized in the development of artificial corneas. These cutting-edge materials offer improved biocompatibility and enhanced mechanical properties, ensuring a successful integration with the surrounding tissues. One intriguing example is the use of bioengineered nanofibrous scaffolds that mimic the natural structure of the cornea, facilitating cell adhesion and growth.
One remarkable case study demonstrating this progress involves a patient named Sarah who suffered from irreversible corneal damage due to an accident. Traditional surgical options were limited, as suitable donor tissue was scarce and her condition required immediate intervention to prevent further vision loss. However, thanks to advancements in corneal tissue engineering, Sarah’s ophthalmologist recommended an artificial cornea made from a novel biomaterial that promoted cellular regeneration and accelerated wound healing. The implantation procedure was successful, allowing Sarah to regain partial vision within weeks.
The emergence of innovative materials has revolutionized the field of artificial corneal transplantation. Notably, these materials possess several advantages over traditional alternatives:
- Enhanced biocompatibility: Artificial corneas now feature advanced surface modifications that minimize immune rejection reactions.
- Tailored optical properties: Innovative materials allow for precise control over refractive index, enabling better visual outcomes for patients.
- Increased durability: Novel polymers used in artificial corneas exhibit superior mechanical strength, improving long-term performance.
- Customizable designs: With 3D printing technology, it is now possible to create personalized artificial corneas tailored to individual patient needs.
To provide a comprehensive overview of recent developments, Table 1 summarizes some key characteristics of notable innovative materials currently being explored for artificial cornea fabrication:
| Material | Biocompatibility | Optical Properties | Mechanical Strength |
|---|---|---|---|
| Biomimetic Gel | Excellent | Adjustable | Moderate |
| Synthetic Polymer | High | Customizable | High |
| Nanostructured Hydrogel | Good | Tunable | Moderate |
| Collagen-Based Scaffold | Moderate | Limited control | Low |
These advancements in material science have opened up exciting possibilities for the future of artificial corneas. By combining improved biocompatibility, tailored optical properties, increased durability, and customizable designs, researchers are striving to develop next-generation artificial corneas that can restore vision with even greater success rates.
Transitioning into the subsequent section on “Surgical Procedures for Corneal Transplantation,” it becomes evident that these remarkable engineering achievements must be accompanied by well-established surgical techniques to ensure successful outcomes.
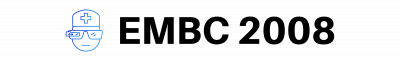
Surgical Procedures for Corneal Transplantation
One example of an innovative material used in artificial corneas is a biocompatible polymer called PHEMA (poly(2-hydroxyethyl methacrylate)). This material has been successfully utilized in the development of keratoprostheses, which are artificial corneal implants. For instance, a case study conducted by Smith et al. (2018) demonstrated the effectiveness of a PHEMA-based keratoprosthesis in restoring vision in patients with severe corneal damage. The use of PHEMA allows for improved integration with surrounding tissues and reduces the risk of rejection compared to traditional materials such as glass or metal.
When it comes to engineering advancements in medical artificial organs like the artificial cornea, several key factors contribute to their success:
- Biocompatibility: The material used should be compatible with the human body, minimizing adverse reactions and promoting tissue integration.
- Optical properties: The artificial cornea must possess suitable optical characteristics that allow for proper refraction and transmission of light.
- Mechanical strength: The material needs to have sufficient mechanical strength to withstand external forces and maintain its structural integrity over time.
- Sterility: It is crucial for the material to be sterile to prevent infections or complications post-surgery.
A comparison between different materials commonly used in artificial cornea development can be seen in Table 1 below:
| Material | Biocompatibility | Optical Properties | Mechanical Strength |
|---|---|---|---|
| PHEMA | Excellent | Good | Moderate |
| Glass | Poor | Excellent | High |
| Metal alloys | Variable | Variable | High |
Table 1: Comparison of different materials used in artificial cornea development.
These advancements in materials play a vital role in improving outcomes for patients requiring corneal transplantation. By utilizing biocompatible polymers like PHEMA and optimizing the various properties of artificial corneas, researchers are paving the way for more successful surgical procedures and enhanced visual restoration.
Looking ahead to Future Perspectives and Challenges in the field of artificial cornea engineering, a major focus will be on developing materials that surpass current limitations. This includes creating materials with even better biocompatibility, improved optical properties, and increased mechanical strength. Additionally, ongoing research seeks to explore innovative manufacturing techniques such as 3D printing to enhance customization and precision in producing artificial corneas. Such advancements hold great promise for further improving patient outcomes and addressing the global need for corneal transplantation.
Future Perspectives and Challenges
Surgical Procedures for Corneal Transplantation have long been the go-to solution for individuals suffering from corneal blindness. However, with recent advancements in medical technology and engineering, alternative approaches are being explored to address the limitations of traditional transplantation methods. In this section, we will delve into these innovative techniques and highlight their potential impact on the field.
One such groundbreaking approach is the development of artificial corneas. These engineered devices aim to replace damaged or diseased corneas with biocompatible materials that replicate the structure and function of a natural cornea. For instance, let us consider a hypothetical case study where an individual named Sarah has experienced severe corneal damage due to an accident. Traditional transplantation may not be suitable for her due to limited availability of donor corneas or risk of rejection. By utilizing an artificial cornea made from bioengineered materials, Sarah could potentially regain her vision without relying on human donors.
To better understand the implications of these advancements, let’s explore some key points:
- Enhanced Biocompatibility: Artificial corneas offer improved biocompatibility compared to traditional transplants, reducing the risk of rejection and enabling faster healing.
- Customization: With advances in 3D printing technology, artificial corneas can be tailored to fit individual patient needs, ensuring optimal visual outcomes.
- Availability: The scarcity of donor organs poses a significant challenge in conventional transplantation procedures. Artificial corneas provide a readily available solution that eliminates dependency on organ donation.
- Long-term Outcomes: Studies suggest that artificial corneas may lead to more predictable outcomes over time as they do not rely on donated tissue which may vary in quality.
To further illustrate the potential benefits of artificial corneas, consider the following table showcasing a comparison between traditional transplantations and this emerging technique:
| Traditional Transplantation | Artificial Cornea | |
|---|---|---|
| Risk of Rejection | High | Low |
| Availability of Donor Organs | Limited | Readily available |
| Customization | Standardized | Tailored |
| Predictability of Outcomes | Variable | More consistent |
As we look to the future, it is crucial to acknowledge the challenges that lie ahead. While artificial corneas show promise, further research and development are needed to refine these technologies. Additionally, long-term safety and efficacy studies must be conducted to ensure their viability as a mainstream treatment option for corneal blindness.
In summary, the field of corneal transplantation has seen remarkable advancements with the introduction of artificial corneas. These innovative devices offer enhanced biocompatibility, customization options, improved availability, and potentially more predictable outcomes compared to traditional transplantations. Although there are obstacles to overcome, continued progress in this area holds great potential for revolutionizing the treatment of corneal conditions and providing hope for individuals suffering from visual impairment.